Move Like You’re Meant To

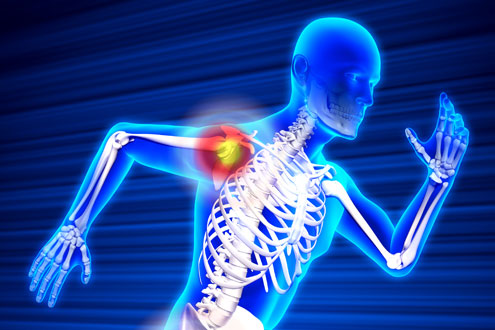
More than half of people over age 50 will experience some form of arthritis – joint pain, aches, and musculoskeletal complaints. Yet, staying active and maintaining a high level of performance into the later years is important for our overall quality of life and mental satisfaction.
In order to understand how to control arthritis, it’s helpful to understand what arthritis is and why it affects so many people. The word “arthritis” comes from the Greek language, and by its own definition means inflammation or disease of the joints.
So what does that really mean?
Our joints are unique due to the presence of cartilage. This connective tissue combines firmness and elasticity to create the lowest friction material. As a result, cartilage allows for super smooth motion with minimum effort. When your joints are young, you can run, jump, and squat without any hint of catching or grabbing in your knee or hip. Unfortunately, as our joints are getting older, cartilage loses some of its capacity to reduce friction. This leads to the joint not moving as smoothly, and causes one of the key symptoms of arthritis: stiffness in the joint.
I like to explain it as a freshly paved asphalt road which is brilliant to drive in the summer and early fall, but is full of potholes after a long winter. Our joints get their own potholes. All the debris from those potholes can cause irritation and inflammation, which doctors call synovitis, and ultimately swelling or effusion. The body is very resilient and usually cleans up the debris, and we get better. Arthritis, however, is a lifelong progressive, chronic condition that is often accentuated by episodic flare-ups. As we get older, we all get some stiffness in the morning and some joint swelling after a day working in the garden; it’s the episodes of pain, catching, and swelling that bring us to the doctor.
If this is your first flare up and you have early arthritis, it will get better before it gets worse.
Here are my best tips:
- Stay active. Exercise can help maintain strength and flexibility. Cartilage does not have its own blood supply and gets nutrition through the fluid movement inside your joint. The best way to then nourish your cartilage is to keep moving, which then swishes the fluid around and makes sure that your entire joint is hydrated. Low impact exercise like walking or swimming are very helpful and focus on motion and flexibility. Such activities can pay dividends in the long run.
- Medication. Take over-the-counter anti-inflammatory medications. A doctor may prescribe ibuprofen, naproxen, or meloxicam in combination with acetaminophen. It’s usually better to take those medications preventively before strenuous activities, rather than playing catchup afterwards when everything is swollen and hurts.
- Physical therapy may also be recommended. Controlled and directed exercise regimens to work on muscle balance, swelling control, and mobility are always super helpful.
- Yoga and tai-chi. These practices have proven over and over to benefit musculoskeletal well-being and relieve joint aches. Some patients say that they cannot do the motions or stretch that far, which is totally fine. There should be no ego involved in exercise. In fact, I see an entire slew of problems derived from exercise in itself, and they often have to do with uncontrolled overzealousness. Instead, focus on good form and balance, appropriate warm up and stretching, and leave out your competitive nature. Only then you can safely progress and improve.
- Exercise. Ultimately, any exercise is better than no exercise. According to many studies, regular physical activity reduces a person’s risk of death from cardiovascular disease, but it is estimated that only half of U.S. adults meet the recommended guidelines of 150 minutes per week of moderate intensity exercise or 75 minutes per week of vigorous intensity exercise. Walking on flat surfaces is healthy and safe. Golf allows you to walk outside, but the irregular unstable grassy surfaces may be tough on your knees, so plan accordingly by perhaps using a brace, taking the cart some, and avoiding hazards. If tennis is your game, consider playing doubles, so the frequency of switchbacks, turns, and rapid stops is reduced. Running is fine, but swimming or bicycling is much better as those sports avoid the constant repetitive full weight impact.
The human body is highly efficient and the dogma “you don’t use it – you lose it” applies to arthritis too. Studies show that cartilage thickness is significantly reduced in animals subjected to prolonged immobilization. In children, articular cartilage volume is increased in association with vigorous physical activity and muscle strength.
So then what causes arthritis? Most studies suggest that osteoarthritis is a result of genetics, nutritional imbalance and obesity, or smoking.
Now I need a knee replacement…
In 2011, over one million total joint replacements were performed in the United States, with that number likely to have surpassed 1.5 million by now. Hips and knees are most common, but also the shoulder, ankle, or finger joints can also be replaced.
Patients generally do remarkably well after such surgery. The surgery itself is about one to two hours, and recovery time gets shorter and shorter, with patients being discharged to home for physical therapy soon after. Total joint replacements may not necessarily save lives, but they do allow for a fun and fulfilling life, all the way into the late 90s.
I am often asked if people living with arthritis can continue playing golf, tennis, and other activities they enjoy. The answer is a definite yes! Living life to the fullest should be our goal, and it can be easily achieved with lifestyle modifications, healthy behaviors, and sometimes the help and direction of a doctor.
If you’re feeling the pains of arthritis, the team at the Total Joint Center can help you. Give us a call so we can help you move the way you’re meant to!

About the Author:
Valentin Antoci, MD, PhD
Valentin Antoci, MD, PhD is chief of the division of arthroplasty at the Brown University Health Orthopedics Institute and The Warren Alpert Medical School of Brown University, and director of the Total Joint Replacement Program at Newport Hospital. He has a particular interest in unicompartmental partial knee replacement, minimally invasive surgery, complex reconstructions, failed total joints, preservation techniques, and trauma.
Find a Doctor

The right provider is in our network
Search more than 1,200 providers in our network.